Look beyond the usual suspects
With a traditional testing approach, clinicians need to choose which respiratory pathogen to test for. COVID-19 testing may be a first choice, followed by influenza. If these tests are negative, additional testing may be required—and at this point, the cost and time involved with serial testing begins to add up.
While COVID-19 and influenza may be top of mind (depending on the season), other respiratory pathogens can be serious as well. For example, every year respiratory syncytial virus (RSV) leads to 58,000 hospitalizations for children younger than 5 and 177,000 hospitalizations for adults 65 and older.1
Adenovirus is another concerning respiratory pathogen. The CDC recently released a health advisory encouraging clinicians who see pediatric patients experiencing acute hepatitis of unknown etiology to consider testing for adenovirus. This comes as the CDC has identified a cluster of children who had hepatitis, some testing positive for adenovirus.2
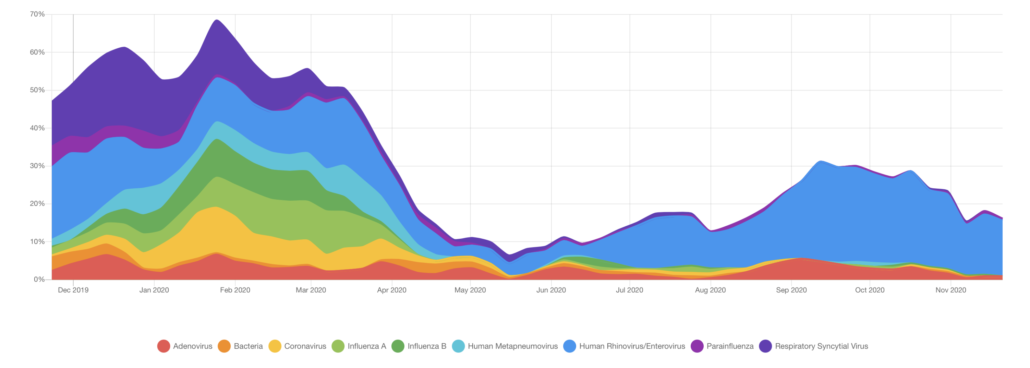
On top of all that, while BioFire® Syndromic Trends showed a decrease in all viral respiratory pathogens in the early months of the COVID-19 pandemic, pathogens like RSV, human rhinovirus/enterovirus, and parainfluenza are again showing a significant percentage of positive detections.3,4 Diagnostics that only test for COVID-19 or influenza may miss these important detections.
Even if the cause is COVID-19 or influenza, rapid tests have lower sensitivity compared with PCR testing. For that reason, the FDA recommends follow-up molecular testing for those who test negative for COVID-19 but are suspected of having COVID-19 due to experiencing symptoms or having recent exposure.5 Follow-up testing can add time and expense to the diagnostic journey.